Nurses Say Pagers Must Go; Hospitals Drag Feet
Nurses and other healthcare workers who communicate vital patient information say they need an alternative to outdated pagers and insecure smartphones.
At most hospitals, nurses are still required to communicate with colleagues and doctors via Voice over IP (VoIP) or pagers. But many nurses, who tend to be constantly on the go, are increasingly ignoring policy and are texting from their smartphones instead. This approach carries risks: Not only are the phones insecure, but they could also introduce germs into sterile environments.
Pagers may be less risky, but they aren't efficient. They cost US hospitals $8.3 billion in 2013, according to a report by the Ponemon Institute: $3.2 billion through time-consuming discharge processes and another $5.1 billion while clinicians waited for patient information (an average of 46 per minutes per day).
Fed up with waiting for pages, nurses are taking matters into their own hands. Although 89% of hospitals forbid the use of personal smartphones at work, 67% of hospitals report nurses are using their iPhones, Androids, and other devices to support clinical communications and workflow, according to a new report by Spyglass Consulting Group. Hospital IT departments know nurses are doing this, but they don't have the time or the resources to monitor their usage. Of the 53% of hospitals with BYOD programs, only 11% include nursing staff.
Hospitals recognize they must improve nursing communications. According to Spyglass, only 4% currently have nursing smartphone systems installed, but 51% are investing in or evaluating these technologies, and half of the more than 100 hospitals surveyed have already implemented VoIP-based systems.
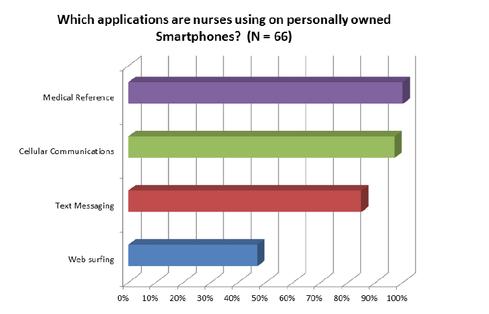
(Source: Spyglass Consulting)
Despite being user-friendly and widely available, consumer smartphones are not designed for hospital use, 89% of respondents told Spyglass. Enterprise-class solutions, especially systems that integrate with EHRs, are rare since hospitals want smartphones to support real-time VoIP, HIPAA-compliant secure text messaging, alerts and alarms approved by the Food & Drug Administration (FDA), simple nursing documentation, and bar code scanning for medication administration. In addition, 88% of survey respondents worried about the risk of mobile devices on their network -- particularly violating HIPAA security and patient privacy rules -- and the danger of introducing viruses and other malware to the network.
But merely giving nurses secure texting capabilities isn't enough, said Dr. Benjamin Kanter, chief medical informatics officer at Palomar Health, in an interview. "Can you make a message that's smart, that can escalate, and can you start to message within the context of a patient's record? The message is only one piece of the puzzle. You've got to provide context and you've got to be able to create action," he said. "Usually for what nurses are trying to communicate in a hospital, something triggering has occurred and most secure texting systems don't take that into account. It's very different in a hospital environment."
When Palomar Medical Center, in Escondido, Calif., opened its doors in August 2012, it featured distributed stations to keep nurses closer to patients. The hospital wants its nurses to be equipped with enhanced communication capabilities and is exploring new tools, like AirStrip One and Sotera's wireless patient-monitoring devices.
Hospitals must improve their communication systems because medicine today involves so many specialists and handoffs, said Dr. Steven Davidson, senior VP and chief medical informatics officer at Maimonides Medical Center in Brooklyn, N.Y. But most currently available tools don't fit all requirements, especially as many hospitals use more than one EHR.
Today, Maimonides allows all clinicians to see which clinicians are in the hospital and how to reach them, a move designed to speed up patient care. In the future, the hospital would like to integrate that information with the EHR so responding clinicians can immediately view patient records rather than looking them up separately, Dr. Davidson said. Later this year, he added, Maimonides will work to develop bedside medication verification that uses a handheld device, probably built off a smartphone.
Written by Alison Diana
Alison Diana has written about technology and business for more than 20 years. She was editor, contributors, at Internet Evolution; editor-in-chief of 21st Century IT; and managing editor, sections, at CRN. She has also written for eWeek, Baseline Magazine, Redmond Channel...Click here to read the full bio.
Click here to read the original article on Information Week.